 Affecting over 8 million people in the United States, psoriasis is a skin condition due to an abnormal autoimmune response that is characterized by inflammation and patches of scaly, itchy skin.
Affecting over 8 million people in the United States, psoriasis is a skin condition due to an abnormal autoimmune response that is characterized by inflammation and patches of scaly, itchy skin.
Psoriasis is sometimes difficult to treat and there are still many misconceptions about the disease. While many common skin irritations have cures, psoriasis is one skin condition that, unfortunately, remains incurable. So, what is psoriasis — and if we can’t cure it, how can we treat it?
We sat down with Dr. Anjali Vekaria, board-certified Dermatologist at The Dermatology Specialists to learn more about psoriasis and get the inside scoop on how we treat this common medical condition.
Psoriasis is an inflammatory disease in which an overactive immune system produces an abnormally rapid increase in cell buildup on the skin’s surface.
Typically, cells grow deep in the skin and rise slowly to the surface over the course of a month. In people with psoriasis, however, the sped-up process may take just a few days. This overabundance of new skin cells forms raised scales and red patches that are often itchy and sometimes painful.
“While the direct cause of psoriasis remains unknown, we do know it is due to an abnormal autoimmune response, and commonly includes a genetic component,” explains Dr. Vekaria.
Typically, the immune system creates white blood cells to fight bacteria and guard against infections. In the case of psoriasis, white blood cells, often called T cells, mistakenly attack the skin.
Some people may be genetically predisposed to exhibiting psoriatic symptoms. If you have an immediate family member with psoriasis, your risk of developing it is greater.
There are different levels of severity with psoriasis: mild, moderate and severe. Mild psoriasis covers less than 3 percent of the body, moderate covers three to ten percent and severe psoriasis covers over ten percent.
Many different factors can trigger symptoms including infections, stress, injuries to the skin (bug bites or scratches), smoking, heavy alcohol use, and vitamin D deficiency.
The National Psoriasis Foundation reports that while psoriasis can develop at any age, it typically develops between the ages of 15 to 35. Around 10 to 15 percent of psoriasis patients are under the age of 10.
The appearance of psoriasis is unique to each individual. Generally, psoriasis symptoms can range from a few localized spots of dandruff-like scaling to vast eruptions that cover large areas of the body. Most types of psoriasis go through cycles that flare up for a few weeks or months at a time, then subside for a while or even go into complete remission.
Some common signs and symptoms include:
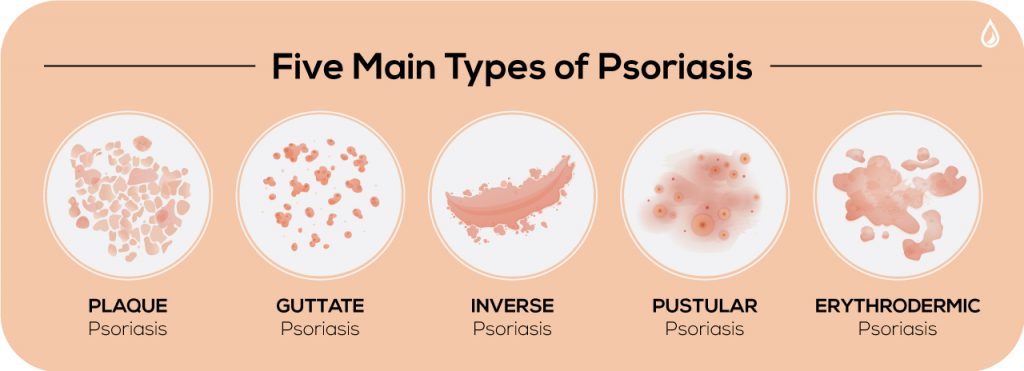
There are five main types of psoriasis which doctors diagnose by the appearance of the skin. Proper identification helps dermatologists and patients more effectively manage symptoms.
Plaque Psoriasis: The American Academy of Dermatology estimates that 80 to 90 percent of people with psoriasis develop this type, making it the most common form. It results in dry, red skin lesions covered in silvery scales. Sometimes the plaques are itchy, painful and can crack and bleed. They can occur anywhere on the body, including the genitals and soft tissue inside the mouth.
Guttate Psoriasis: Common in children and young adults, guttate psoriasis causes small pink spots and generally shows up on the torso, arms and legs. Unlike plaque psoriasis, these spots are not raised or thick. Guttate is the second most common form of psoriasis; nearly ten percent of those with psoriasis develop it.
Inverse Psoriasis: Inverse psoriasis is characterized by bright, inflamed areas with red, shiny and smooth skin. Patches develop under the armpits or breasts, in the groin or around skinfolds in the genital region. It may be triggered by fungal infections.
Pustular Psoriasis: Commonly found in adults, pustular psoriasis causes white, pus-filled blisters and broad areas of red and inflamed skin. It’s localized to smaller areas of the body like the hands or feet, but it can become widespread.
Erythrodermic Psoriasis: This is an extremely rare and severe form of psoriasis, often covering large areas of the body at once. The skin looks similar in appearance to a sunburn; scales develop and can slough off in large sheets. It’s often painful and itchy. Patients with erythrodermic psoriasis typically run a high fever or become very ill. This form can be life-threatening so patients should see a doctor immediately.
Psoriasis can also affect more than just the skin. It can have a wide range of health complications and increase the chances of certain diseases.
“If untreated, one of the most serious complications patients can develop is psoriatic arthritis, causing joint damage and loss of function, which affects approximately a third of psoriasis patients,” says Dr. Vekaria.
Psoriasis patients also need to be careful with their diet and watch for fluctuations in their weight. The disease is known to increase obesity, high blood pressure and type 2 diabetes. For the latter, the risk becomes greater as the severity of the psoriasis increases.
Other conditions to be mindful of include cardiovascular diseases and autoimmune diseases like celiacs, sclerosis and an inflammatory bowel illness known as Crohn’s disease. Moderate to severe psoriasis has also been linked to a higher risk of kidney and Parkinson’s as well.
Of course, patients also need to take care of their mental health as they manage their symptoms. Psoriasis often affects a patient’s quality of life and is associated with low self-esteem, depression and withdrawal from social life.
While this can all sound overwhelming, there are many effective ways to treat psoriasis in its various forms.

Although chronic psoriasis symptoms are manageable in most cases, lifestyle measures including moisturizing, quitting smoking and managing stress can help patients more effectively maintain a normal daily routine.
Dr. Vekaria says, “Being evaluated by a medical professional for your skin conditions can help determine the best types of treatment for you. Sometimes, one treatment type may be better than others, so working closely with your physician can be very helpful in achieving optimal therapeutic results.”
Diagnosis is fairly straightforward. First, a dermatologist determines what type of psoriasis you have, its severity and your personal preference of treatment options. Your doctor will also need to know your medical history to see if you have any concomitant conditions that may affect your psoriasis. The next step is to treat the inflammation and clear the skin. There are three main areas of treatment options:
Topical Treatments
For mild to moderate cases, a dermatologist’s first approach is usually topical over-the-counter or prescription creams and ointments. Topical corticosteroid, calcineurin inhibitors and retinoids, for instance, are prescribed to reduce inflammation and relieve itching. Vitamin D, Anthralin and salicylic acid are treatments that slow skin cell growth while smoothing the skin. If the disease is more severe, creams will likely be combined with oral medications or light therapy.
Light Therapy
Also called phototherapy, light therapy treatments use natural and artificial ultraviolet A (UVA) and ultraviolet B (UVB) light to treat psoriasis either alone or in tandem with medications.
The simplest light therapy option involves exposure to natural sunlight to slow skin cell turnover and inflammation. Controlled, daily exposure to small amounts of the sun’s UV rays can improve psoriasis, though prolonged amounts can cause sunburn which only further damages the skin.
Dr. Vekaria explains, “If psoriasis resists topical treatments or natural sunlight, UVB phototherapy could be a good option for those patients looking to treat their psoriasis with a traditional method and minimal side effects like itching, redness or dryness.”
She continues, “These in-office treatments involve controlled doses of UVB light usually multiple times a week under supervision from a dermatologist to treat widespread psoriasis patches that are mild to moderate in severity.”
Narrow band UVB phototherapy is another form of laser therapy. It’s sometimes more effective than broadband UVB treatment and is generally applied two to three times a week until the skin shows improvement. Afterward, follow-up appointments may be required only once a week. However, patients might experience side effects like severe scarring or long-lasting burns, so it’s important to weigh the pros and cons of undergoing this therapy with your dermatologist.
Excimer lasers are another option used to treat mild to moderate psoriasis, targeted only at the areas with psoriasis without harming healthy skin. A UVB light is directed onto psoriasis plaques to control scaling and inflammation. This treatment uses more powerful UVB light, so it requires fewer sessions than traditional phototherapies.
A more aggressive treatment, psoralen plus ultraviolet A (PUVA), involves patients taking light-sensitizing medication (psoralen) before they’re exposed to UVA light, which penetrates deeper than UVB light. It’s been consistently proven to improve psoriasis and is also used for severe cases. Short-term side effects may include nausea, headaches, burning or itching. Potential long-term side effects include wrinkled skin, freckles, and increased sun sensitivity with greater risks of skin cancer.
Oral or Injected Medications
For some patients, psoriasis (ranging anywhere from mild to severe forms) sometimes doesn’t respond well or is resistant to other treatments. In this case, oral or injected medications are often the next step in treatment. However, doctors may only prescribe these medications for a brief amount of time or alternate them with other forms of therapy as medications can sometimes have negative side effects on the body.
Apremilast is a common medication for patients with mild symptoms. For those with more serious cases, typical medications include acitretin, methotrexate, cyclosporine, and biologics (like Stelara and Enbrel).
Biologics are some of the newest and most popular options on the market. These medications target parts of the immune system that are responsible for the inflammatory process causing psoriasis. There are many different types of biologics available depending on the presence of psoriatic arthritis or any concomitant health conditions.
Currently, many biologics are offered as injections, and are generally used for people who do not respond well to traditional medications or for those with associated psoriatic arthritis.
Dr. Vekaria says, “Biologics have specifically shown great promise since it is a targeted form of treatment with fewer side effects than other traditional ones. New biologics continue to be tested to achieve treatments with the fastest and most effective response rates for disease clearance, all with good safety profiles.”
Psoriasis shouldn’t have to infringe upon your life. Although it can be a frustrating skin condition to live with, there are now several medications and sophisticated treatments that can help ease symptoms and manage the disease.
Ongoing clinical trials are leading to even more effective therapies, and with so many advancements in the field, patients who deal with psoriasis have an opportunity to more effectively manage their symptoms.
Luckily, through an active therapy regime and the support of a dermatologist, psoriasis and its sudden outbreaks no longer have to be an enigma for patients. Though psoriasis remains technically incurable, new advancements offer an optimistic future that keeps getting better for people with the disease, offering them opportunities to break free from the pain, irritation, or even social stigma which may have otherwise burdened them in the past.
 Anjali S. Vekaria is a board-certified dermatologist at The Dermatology Specialists. She received her bachelor’s degree from the University of Georgia, her medical degree from the Medical College of Georgia, and completed a research fellowship and dermatology residency at the Icahn School of Medicine at Mount Sinai. Dr. Vekaria has overseen 40+ clinical trials for new medications treating skin conditions like eczema and psoriasis and has authored several peer-reviewed articles in her field.
Anjali S. Vekaria is a board-certified dermatologist at The Dermatology Specialists. She received her bachelor’s degree from the University of Georgia, her medical degree from the Medical College of Georgia, and completed a research fellowship and dermatology residency at the Icahn School of Medicine at Mount Sinai. Dr. Vekaria has overseen 40+ clinical trials for new medications treating skin conditions like eczema and psoriasis and has authored several peer-reviewed articles in her field.